Medicare Part C
Medicare Advantage Explained
Medicare Advantage plans were created as an alternative to Original Medicare and Medigap. By joining one of these plans, you direct Medicare to pay the Advantage plan a set monthly amount for your care. In return, the plan will deliver all of your Part A & Part B services. They take on all of your medical risks.
You must continue to pay your Medicare Part B premium while enrolled in an Advantage plan. You must be enrolled in both Medicare Parts A and B and live in the plan’s service area.
Medicare Advantage policies are NOT Medigap plans. They work differently because they pay instead of Medicare, not after Medicare.



Medicare Advantage Coverage VS Original Medicare
Many people new to Medicare will ask us about the pros and cons of Medicare Advantage plans vs Original Medicare. Much of this is in the way you access your benefits.
With Original Medicare, you will have deductibles and a 20% coinsurance on Part B. You can visit any doctor or hospital that participates in Medicare, and most do.
With an Advantage plan, you will use the plan’s network of providers, which is usually local. You will pay co-payments when you receive healthcare services. Each plan sets its own cost-sharing. For example, you might pay a small copay for a primary care doctor visit and perhaps a higher copay to see a specialist. Likewise, some plans will charge you a daily hospital copay, and other plans might charge a flat amount for the whole stay.
Perhaps one of the biggest differences is in changes to the plans. Medicare may have small changes to the Part A and B deductible, but the 20% coverage on outpatient services never changes. Part C Medicare Advantage plans change annually.
Why Medicare Advantage was Created?
For many years, people on Medicare had only Medigap plans to choose from. While these plans have excellent coverage, not everyone can afford them. These people often opted to have only Original Medicare. When illnesses struck, they would find themselves with bills for expensive deductibles and coinsurance that they could not afford.
At this time, they might try to get a Medigap plan, but now that they have developed health issues, they could not qualify. This often resulted in medical bankruptcy.
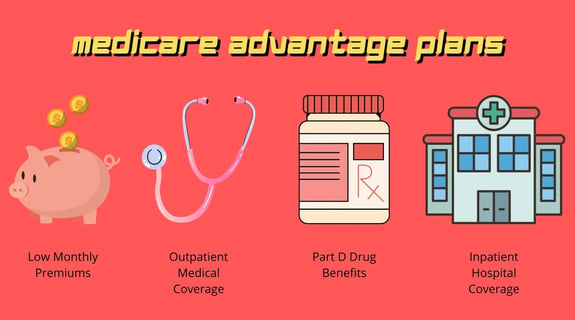
Medicare Part C plans provide a solution to these problems. Medicare Part C provided lower-cost plans with just one health question. People can now join them during certain times of the year, called enrollment periods.
Advantage plans were also built with an out-of-pocket maximum cap on your medical spending. Think of this as a safety net. If you have heavy health spending that results in a certain out-of-pocket limit, then the plan kicks in and pays the rest for the remainder of the calendar year (Part D expenses are calculated separately).
Another popular feature of Advantage plans is that they often include a built-in Medicare Part D drug plan, which saves you from having to purchase that separately.


Joining an Advantage Plan
If you are trying to decide which type of coverage is appropriate for you, the best option is to do your research. As always a professional agent can educate you on Medicare Advantage vs Medicare Supplement coverage. Medicare Advantage can be explained in comparison to Medigap as your other option.
Part C Advantage plans have different networks, premiums, and cost-sharing. Working with an insurance agency that specializes in these plans is a great way to ensure that you consider all the variables before choosing your insurance company. Kim Youngs is very familiar with how Medicare Advantage plans work. Want Medicare Advantage explained in a one-on-one setting? Get help from our Medicare insurance expert today at 816-436-9977!

How Medicare Advantage Works
A Medicare Advantage plan is a private Medicare insurance plan that you may join as an alternative way to get your Part A and Part B benefits. When you do, Medicare pays the plan a fee every month to administer your Part A and B benefits.
You must continue to stay enrolled in both Medicare Part A and B while enrolled in your Medicare Advantage plan. Medicare pays the Advantage plan company on your behalf to take on your medical risk. This is how Medicare Advantage plans are funded.
You will present your Advantage plan ID card at the time of treatment. Your providers will bill the plan instead of Original Medicare. Again, this is also why some providers consider them Medicare replacement plans, but it’s important to remember that you can always return to Original Medicare during a future annual election period.
Medicare Advantage Summary Of Benefits
Each Advantage plan has its own summary of benefits. This summary will tell you what your copays will be for various healthcare services. Your plan will offer all the same services as Original Medicare, such as doctor visits, surgeries, lab work, and so on.
You might pay $0 to see a primary care doctor. Specialists will often be more – a $25 specialist copay is quite common. Some of the higher copays may come in for diagnostic imaging, hospital stays, and surgeries.
You can usually expect to spend several hundred on copays for these items. However, this varies greatly between states, so review plans in your area to get the specifics.
One neat thing about Medicare Advantage plans is that some of them offer minor benefits for routine dental, vision, or hearing. Some plans include gym memberships.
When searching for Medicare Advantage plans with dental and vision, our experts here at Kim Youngs Agency can help you compare those ancillary benefits between carriers.


Medicare Advantage Network
In exchange for lower premiums that Advantage plans offer, you agree to play by certain rules. Most Medicare Advantage plans have HMO or PPO networks.
Medicare HMO Networks
Medicare HMO networks are generally required to treat only with network providers, except in emergencies. You will usually need to select a primary care physician. That physician can coordinate a referral if you need to see a specialist. There are some HMO plans that offer a point-of-service feature where you can see out-of-network providers in certain circumstances.
Medicare HMO plans are the most prevalent type of network. According to a study by Mark Farrah Associates, they will represent 71% of all Medicare Advantage plans on the market.
Medicare PPO Networks
Medicare PPO networks allow you to see doctors outside the network but you’ll have substantially higher out-of-pocket spending to do so.
In limited counties, there are Medicare Private-Fee-for-Service plans. These plans may or may not include Part D. How you access care is also different. While this plan type was very common in the past, it has been slowly phased out in most areas.
You can learn more about Medicare PFFS plans by getting in touch with a knowledgeable professional agent like Kim Youngs at 816-436-9977 or doing research on your own.
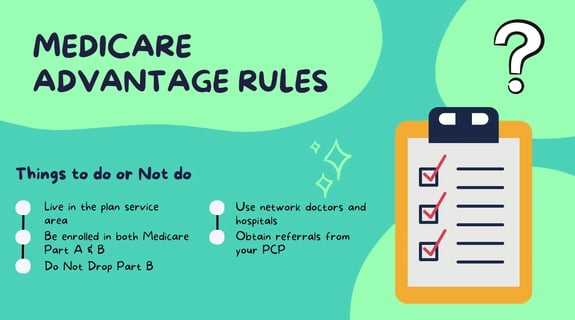
Basic Medicare Advantage Rules
If you are deciding between Medicare Advantage and Medigap, you’ll want to consider some of the rules before you enroll.
You must be enrolled in both Medicare Part A & B and live in the plan service area. Some people think they can drop Part B if they enroll in Medicare Advantage. That is incorrect If you drop Part B while enrolled, you will immediately be disenrolled from your Medicare Advantage plan.
Use network doctors and hospitals for the lowest out-of-pocket costs. Plans may have HMO or PPO networks. Most Medicare HMO plans do not cover anything out of network except emergencies. In PPO networks, seeing a provider outside the network will result in higher spending for you.
Advantage plans may require prior authorization for certain procedures
You may need to obtain a referral from your primary care physician before seeing a specialist on many HMO plans
Put your red, white, and blue Medicare card in a safe place. Do not give it to any of your healthcare providers. If they bill Medicare, those bills will be rejected because they should have been sent to your Medicare Advantage insurance company for processing.
You must direct your providers to bill your Medicare Advantage plan. People who enroll in Advantage plans for Medicare are agreeing, for the rest of the calendar year, to be covered by the plan instead of Original Medicare.
Medicare Advantage Enrollment Periods
Medicare Advantage plans have lock-in periods. You can enroll in one during the Initial Enrollment Period when you first turn 65. After that, you may enroll or dis-enroll only during certain times of the year. Once you enroll in Medicare Advantage, you must stay enrolled in the plan for the rest of the calendar year. You may only dis-enroll from an Advantage plan during certain times of the year unless you qualify for a special enrollment period due to a specific circumstance.
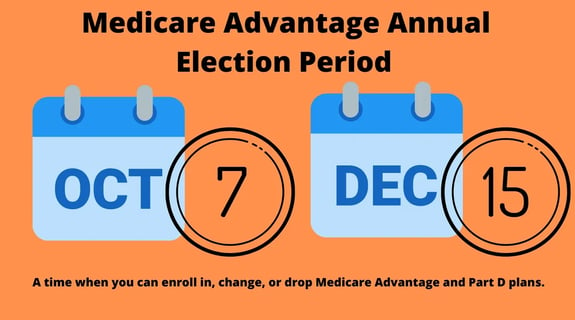
The Annual Election Period in the fall is the most common time to change your Medicare Advantage plan. This period runs from October 15th – December 7th each fall. Changes made to your enrollment will take effect on January 1.
If you decide to leave a MAPD and return back to Original Medicare, you must notify your Medicare Advantage plan carrier. Otherwise, Medicare will continue to show that you are enrolled in the Advantage plan instead of Medicare.
Medicare Advantage Open Enrollment Period
Some people join Medicare Advantage plans without doing any research about how these plans work or speaking with an agent who can advise them. Therefore they don’t know about all of these rules. They may find themselves enrolled in a plan that their doctor doesn’t accept or that doesn’t include one of their medications. This happens most often in January after a person has used the Annual Election Period to join a Medicare Advantage plan.
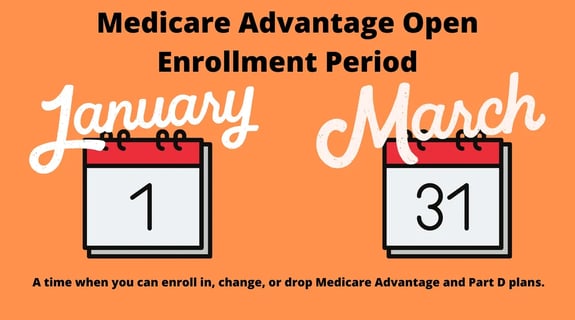
For this reason, Congress designed the Medicare Advantage Open Enrollment Period that runs from January 1st – March 31st each year. During this time, you can disenroll from any Medicare Advantage plan and return to Original Medicare. You will be allowed to add a standalone Part D drug plan.
Unfortunately, this does not guarantee that you can return to the Medigap plan you had before. Unless this was your first time ever in a Medicare Advantage plan, then you will usually have to answer health questions and go through medical underwriting to get re-approved for Medigap. Consider this before dropping any Medigap plan to go to Medicare Advantage.
Your other option during the Medicare Advantage Open Enrollment Period is to change from your current Medicare Advantage plan to a different Medicare Advantage plan. Please be aware that you can only use this period once per calendar year.